
Inflammatory Bowel Disease (IBD) is a broad term that describes conditions with chronic or recurring immune response and inflammation of the gastrointestinal tract.
CDC
Inflammatory bowel disease (IBD) involves chronic inflammation of all or part of your digestive tract.
Mayo Clinic
IBD stands for Inflammatory Bowel Disease. The two most common forms are Crohn’s Disease (often just called Crohn’s) and Ulcerative Colitis (UC). In both UC and Crohn’s parts of the digestive system (the gut), which includes the intestines or ‘bowels’, become sore and inflamed.
CCUK
Table of Contents
What is IBD?
Pretty much everyone agrees that IBD is a term used to describe chronic inflammation of the digestive system.
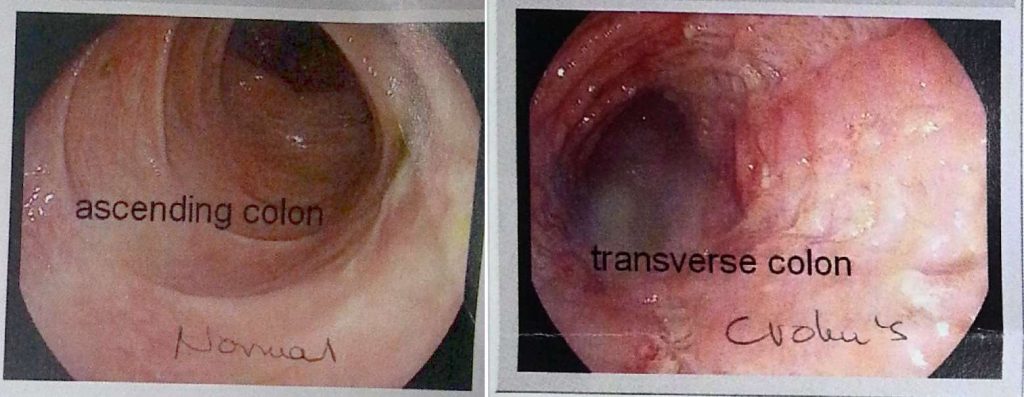
You will find both Crohn’s Disease and Ulcerative Colitis under the IBD umbrella, and while someone with either disease may have similar symptoms, the location and presentation of these two are often quite different.
It’s been estimated that there are over 5 million people living with IBD worldwide, and Canada has among the highest rate per capita.
IBD (Inflammatory Bowel Disease) is not the same as IBS (Irritable Bowel Syndrome).
Here is a quick (and incomplete) comparison between Crohn’s Disease (CD) and Ulcerative Colitis (UC). Please note that not all symptoms will manifest in every person, and the severity of these symptoms can also vary wildly from person to person.
| Crohn’s Disease | Ulcerative Colitis | |
|---|---|---|
| Location | Anywhere from “mouth to anus”; most often in small intestine | Colon and often rectum |
| Distribution | Inflammation is often patchy; referred to as skip lesions | Inflammation is usually continuous |
| Depth of inflammation | Can penetrate through the bowel wall | Tends to only affect the lining (“mucosa”) |
| Common symptoms | Fever | Fever |
| Abdominal Pains | Abdominal Pains | |
| Joint pains | Joint pains | |
| Diarrhea / constipation | Diarrhea / constipation | |
| Bowel urgency | Bowel urgency | |
| Fatigue | Fatigue | |
| Weight Loss | Weight Loss | |
| Nausea / vomiting | Nausea / vomiting | |
| Anemia | Anemia | |
| Inability to absorb nutrients | Nutrient malabsorption can happen, but not as common since the colon isn’t responsible for the absorption of key nutrients. | |
| “Extraintestinal manifestations” | It happens | You bet |
| Bloody stool? | Not often, although if the disease is active in the colon and/rectum (as it was for me), then rectal bleeding can happen. | Yup |
| Fistula / abscesses? | Common | Nope |
| Strictures (narrowing of the bowel wall) | Yes, ma’am! | Yes |
Who gets IBD?
Teens and young adults are more likely to be diagnosed with IBD, although it can be diagnosed in the very young and older folks too (SOURCE).
It seems that IBD is also a bit of a racist too, targeting whites and certain Jewish populations more than any other race or group of people (SOURCE).
IBD also hates developed nations, apparently, and incidences tend to be higher in places like Canada, the United States and Europe; researchers are still trying to find out why this is the case, but there is speculation that it could be linked to changes in diet, environmental exposure and even changes in bacteria from one place to another (SOURCE).
What Causes IBD?
Unfortunately, we don’t know what exactly causes IBD, despite what everyone and their brother seems to think, but researchers are looking at possible genetic links and environmental triggers that could explain how and why someone develops IBD.
Some researchers suggest that an imbalance in our gut bacteria triggers an inappropriate immune response that ends us damaging our gut, while others believe that something in the environment has flipped a switch in our genes that create an autoimmune response (SOURCE).
While the research is still new and ongoing, I find it fascinating to hear about new theories as more and more data is collected and analysed.
Something that I’ve always found interesting is reading about how IBD can affect twins, specifically, when one of the twins gets IBD and the other doesn’t; to me, this seems to suggest that environmental triggers are highly relevant, even though genes can obviously play a role (SOURCE).
What Are the Risk Factors for Ibd?
Because we don’t know the cause of IBD (yet), we can only estimate risk factors between certain behaviors, environmental exposure, and genetic disposition.
I’ve written several posts about these risk factors HERE and HERE, but it can’t be stressed enough that these risk factors have not been proven as definitive causes or triggers for IBD.
Still, I do believe they offer valuable insight that reinforces the need to eat healthfully, exercise, not smoke and not overusing certain prescription drugs.
It shouldn’t surprise anyone that the risk factors we see for IBD are similar to the risk factors we see for just about any other chronic illness.
Is There a Cure?
Right now, we’re SOL on a cure (and no, the removal of our bowels is NOT a cure!), but we do have several treatment options that range from steroids and anti-inflammatory drugs to immunosuppressants and biological drugs (Remicade, Humira, Entyvio, etc).
There are other treatment options being studied, like FMT (Fecal Microbiota Transplantation), medicinal cannabis, anti-MAP vaccines and stem-cell therapy, but these therapies are experimental and research is ongoing.
For most people with Crohn’s Disease, surgery will happen at some point to remove a part of the bowel, and in some cases, like my own, an ostomy is required.
Some people who have Ulcerative Colitis may be a candidate for an ileostomy or even an internal pouch, like a J-Pouch or K-Pouch, but this isn’t always guaranteed as risk-free and many will still experience extraintestinal manifestations or complications with their internal pouch.
References
- World Gastroenterology Organisation Global Guidelines. Inflammatory bowel disease: a global perspective
- Naser SA, Sagramsingh SR, Naser AS, Thanigachalam S. Mycobacterium avium subspecies paratuberculosis causes Crohn’s disease in some inflammatory bowel disease patients. World Journal of Gastroenterology : WJG. 2014;20(23):7403-7415. doi:10.3748/wjg.v20.i23.7403.
- Spehlmann ME, Begun AZ, Saroglou E, Hinrichs F, Tiemann U, Raedler A, Schreiber S. Risk factors in German twins with inflammatory bowel disease: results of a questionnaire-based survey. J Crohns Colitis. 2012 Feb;6(1):29-42. doi: 10.1016/j.crohns.2011.06.007. PubMed PMID: 22261525.
Further Reading
- Crohn’s and Colitis Foundation: The Facts About Inflammatory Bowel Disease
- Crohn’s and Colitis Canada: What are Crohn’s and colitis?
- Crohn’s and Colitis UK: What is IBD?
Very good overview. Thank you.