Anyone with an ostomy will tell you that sometimes their stoma will often act as if it has a mind of its own!
In this article, I’ll be explaining why stomas move, shrink, and grow!
Table of Contents
Video
This video is brief, but it touches upon some of the major reasons why our stomas may change their shape.
By playing the above video you agree to YouTube's Terms and Conditions and Privacy Policy
What’s Going On?!
It can be alarming to some and amusing to others, but there are several reasons why your stoma might move around and change size.
Some of these reasons are totally natural and should not worry you, and others may need surgical intervention to correct.
Reduction in Swelling After Surgery
Surgery is traumatic for the body, and it’s completely normal to have a swollen stoma soon after surgery.
If you measure your stoma, you may notice that it shrinks for the first 6 weeks or so after your surgery (with the most noticeable change happening in the first week). This is completely expected, and it’s the main reason why patients are asked to measure their stoma before each appliance change for the first little while post-op.
At the same time, it’s often not wise to keep your appliance on for more than a few days in the month following your surgery, as it may lead to leaks and skin irritation as the hole becomes too large for your changing stoma.
This happened to me when I tried pushing my wear time to a week while my stoma size was still in transition – it was a painful lesson that I hope nobody repeats.
There is no exact time frame for when your stoma will reach a consistent size, and you may find yourself having to measure your stoma months or years after your surgery (like I do) because of various factors.
Peristalsis
One of the most common reasons why your stoma would change size and shape is peristalsis.
Peristalsis is a natural, wave-like movement of your intestines caused by muscle contractions in your gut. It serves an incredibly useful function of getting stool through your system and without normal peristalsis you may develop motility issues.
It’s important to realize that peristalsis is not something you can control; it’s like a heartbeat, so your body will know exactly when it should happen (unless you have a motility disorder).
Because a stoma is part of your intestine sticking out of your body, you might be able to see peristalsis in action whenever a bowel movement happens. This is actually one of the reasons why I like wearing clear ostomy bags – it’s interesting to see it in action!
Sometimes, it’ll look like your stoma is getting bigger, while other times your stoma may appear as if it’s retracting or getting smaller. Either case is normal, however, I tend to notice that my stoma will retract more with peristalsis when I have a partial blockage (you may notice this, too).
When cutting a hole for your appliance, always remember to make the hole slightly larger (only by a few millimeters) to account for peristalsis making your stoma larger.
While peristalsis on its own does not (and should not) cause you pain, you may notice sharp pains coming in waves around your stoma if your wafer is cut too small.
Likewise, you may also feel waves of pain caused by peristalsis if you have a blockage.
Weight Loss / Weight Gain
Whether you’re experiencing intentional weight gain/loss or if it came about due to illness or other factors, it can still cause your stoma to change size or shape.
Many of us experience dramatic changes in our weight after surgery, so it goes without saying that we may also find our stomas changing with the rest of our body.
If you use pre-cut wafers and are planning to go on a diet, be sure to keep this in mind as the hole in your wafer may no longer fit your stoma properly.
Along with our stoma changing size, weight loss/gain may also cause our skin to stretch our develop folds which can cause our wafers to no longer give us a good seal.
Always keep these things in mind so you can plan for them.
Flush or Retracted Stoma
Most normal stomas stick out a little bit, but some people may have what’s called a “flush” or “retracted stoma”.
In the case of a flush stoma, there is very little or no bump and the stoma is flat with the skin.
For a retracted stoma, the stoma actually points inwards, and this can be an ongoing problem for some ostomates. The cause of a permanent or chronically retracted stoma is often linked back to poor stoma placement.
Both a flush and retracted stoma can cause issues like leaks or poor appliance adhesion, and in some cases, a surgical revision needs to be made to correct it.
For me, having a blockage (whether it’s a partial or complete obstruction) causes my stoma to shrink and retract. In fact, it’s one of the red flags I use to warn me of blockages-in-progress, and it may be something you notice too.

This happens temporarily and my stoma returns to normal once the blockage is resolved.
Prolapsed Stoma
The opposite of a retracted stoma is a prolapsed stoma.
There are two types of stoma prolapse, one that is “fixed” and one that is “sliding”.
A fixed prolapse is usually caused by the stoma not being created properly while the sliding type can happen for various reasons.
Seeing a prolapsed stoma can be alarming and some extend out over 6″, which can cause problems fitting an appliance and can reduce a patients quality of life.
Someone who has a prolapsed stoma may experience it at random times, and this can make measuring the stoma more challenging.
Unless a prolapsed stoma is causing dangerous complications (like bowel strangulation), the surgical correction is often planned and not urgent (1).
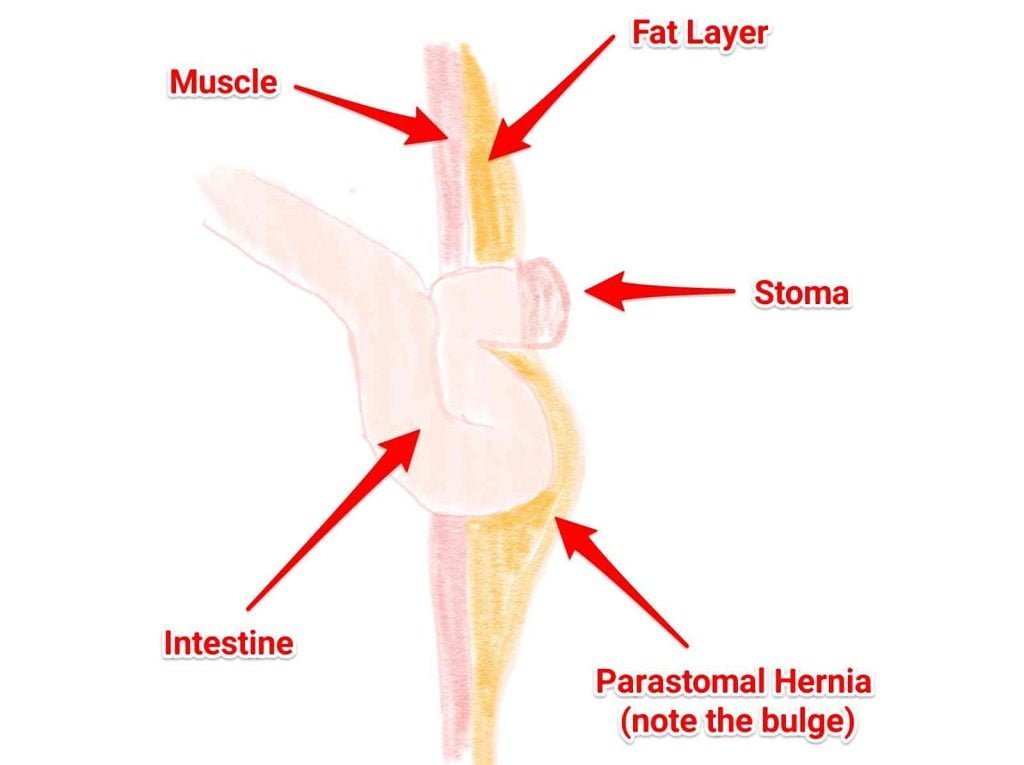
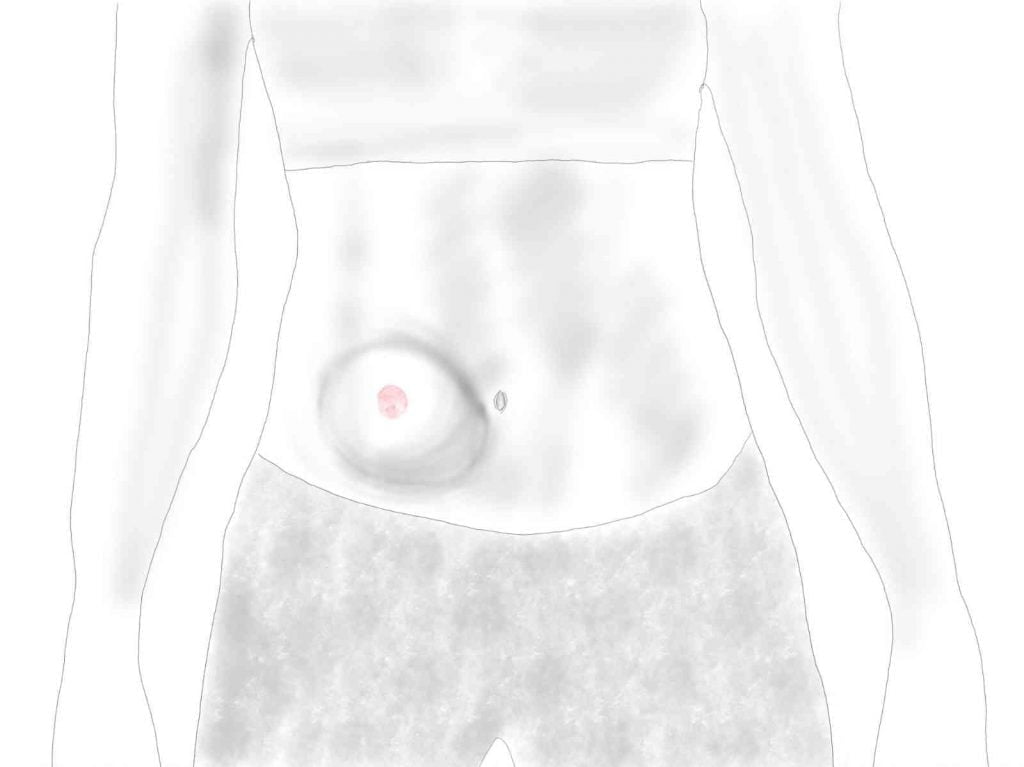
Hernias
Parastomal hernias are caused when a part of your bowel pushes through the muscle wall of your abdomen and can affect a very large percentage of ostomates.
Hernias cause bulges under the skin that can change the size or appearance of your stoma.
Many hernias in ostomy patients are repaired surgically or supported using specialized hernia belts.
Unfortunately, recurrence of hernias is quite high following surgical repair (2) and every new surgery puts a patient at risk of developing one (since the integrity of the abdominal wall is compromised with surgery).
It’s best to consult with a stoma nurse if you have a parastomal hernia because it’s important to manage it in some way to prevent it from worsening.
Pregnancy
As one observant reader mentioned, pregnancy can have an effect on the size, shape, and location of a stoma! (Thanks, Laura!)
These changes are normal and are more common in the second and third trimester. Regardless, the rapid changes to your body can cause difficulties in managing your appliance.
If you do become pregnant and have an ostomy, I would suggest working with both a stoma nurse and an obstetrician so that both your baby and stoma are being looked after :)
My good friend Stephanie Hughes from the Stolen Colon has detailed some of the other changes she’s experienced during pregnancy with an ostomy on one of many articles.
Tips to Manage a Changing Stoma
Here are a few general guidelines for dealing with a stoma that’s not staying a consistent size or shape.
- Measure your stoma. The reason why I like cut-to-fit appliances is that it doesn’t matter what size or shape your stoma is because you’ll be creating the hole yourself. But in order to get the best fit, you should be measuring your stoma before each appliance change (or whatever frequency makes sense to you). If you’re using pre-cut products, I would suggest measuring before placing any new orders, just in case the size is different from what you’ve used previously.
- Try moldable products. If cut-to-fit and pre-cut appliances aren’t working out for you, consider using a moldable appliance. These allow you to fit the wafer around your stoma and then shape it without needing to measure or cut anything.
- Expect change. No stoma will be exactly the same size and shape for a person’s entire life. Knowing that your stoma will change can help you to plan things out and make it less likely to be a surprise when it happens.
- Manage your parastomal hernia. A parastomal hernia can change the landscape of a person’s abdomen, and one that isn’t properly supported or corrected can make ostomy life very inconsistent. Speak with your nurse if you’re having difficulties.
- Learn to “read” your stoma. Our stomas can often give us clues as to what’s going on inside. If you know that your stoma prolapses when exercising or retracts when you have an obstruction, you have an opportunity to prevent these things from happening. You may still need to consult a nurse or surgeon for help, but learning how to “read” your stoma is a great way of providing information that can help them to come up with a plan.
- Don’t take it personally. You may be experiencing a lot of anger or frustration over your shape-shifting stoma. Know that it’s not your fault, but it is something you can learn to manage and work around. The more experience we have with taking care of our stoma, the better we get at anticipating and solving these challenges.
Closing
As you can see, there are plenty of few reasons why a stoma may change shape or size.
A few of these things are in our control, but if you are having continued difficulties with a stoma that’s irregular or changes dramatically then I would highly recommend consulting with a stoma nurse to help you come up with a plan.
I hope that some of the suggestions I’ve offered are helpful, but please let me know if you have any other tips to share.
References
- Kim JT, Kumar RR. Reoperation for Stoma-Related Complications. Clinics in Colon and Rectal Surgery. 2006;19(4):207-212. doi:10.1055/s-2006-956441.
- Gillern S, Bleier JIS. Parastomal Hernia Repair and Reinforcement: The Role of Biologic and Synthetic Materials. Clinics in Colon and Rectal Surgery. 2014;27(4):162-171. doi:10.1055/s-0034-1394090.



I had my bladder removed 12 ago but I see that my stomach is not like a cherry but looks greyish and has shrunk! No other problems! I am now 82 years old! My stomach is not an outie but looks like it has sunk!
Hi Sandie,
It sounds like you might want to ring up your doctor or stoma nurse to have a look at it. The stoma should always look like a healthy, reddish color.
Anytime I try to eat anything besides soft foods the foods tend to get stuck at the stoma and will cause blockage is there anything I can do so I can eat meats and potatoes and regular foods once again because the only thing I am able to eat right now is pudding, apple sauce, and protein drinks please help me I am despite
Hi Jamie,
When did you have your surgery and do you have an ileostomy or colostomy?
Blockages can be common for some people, but there are quite a few variables involved.
I do have several articles that deal with blockages and diet, which may be helpful, but I do suggest speaking with a stoma nurse or your surgeon to discuss this.
Good luck.
I laminated one of my paper measures, worked until I flushed it down the toilet.
Haha! Whoops! ?